Ramp lesions of the medial meniscus.
Ramp lesions of the medial meniscus:
They CAN be seen and fixed from the front of the knee
(with the right techniques and the right kit!)
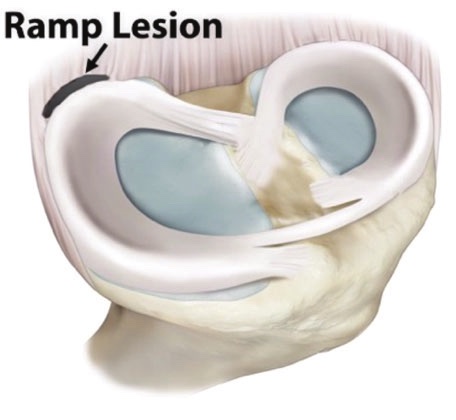
A ramp lesion is a tear around the periphery of the posterior horn of the medial meniscus, with a detachment of the meniscus from the posterior capsule (a tear of the meniscotibial ligament). Ramp lesions were first described by Strobel, back in 1988.[Ref 1] Ramp lesions normally occur specifically in association with ACL tears. They are, however, often missed on MRI and they can also easily be missed intra-operatively, unless the posterior horn of the meniscus is inspected and probed very carefully. It has been estimated that ramp lesions may actually occur in up to 17% of all ACL tears.
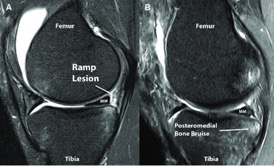
Ramp lesions can sometimes be seen on MRI, either directly, as a clear separation of the posterior horn of the medial meniscus from the adjacent capsule, with a gap visible, or indirectly, through the presence of subchondral bone bruising towards the posterior aspect of the proximal tibia.
Missed / untreated ramp lesions can cause ongoing symptoms after ACL reconstruction, such as medial / posterior pain (particularly with deep flexion), reduced flexion range, pain with impact / twisting, inability to progress appropriately with post-op ACL rehab and reduced end function. Cadaveric studies have also shown that ramp lesions can affect the biomechanics of the joint, increasing anterior and rotatory laxity, particularly in the ACL-deficient knee.
The key to picking up ramp lesions is to have a high index of suspicion and to look carefully and properly when performing the initial arthroscopic evaluation of the joint at the time of ACL reconstruction.
Some people have suggested that ramp lesions can only be diagnosed confidently and accurately by inspecting the posterior aspect of the posterior horn of the medial meniscus via an accessory posteromedial portal. Sonnery-Cottet reported that among 125 tears of the medial meniscus associated with an ACL rupture, 40% were ramp lesions; of these, most (58%) could be detected during exploration of the posteromedial compartment through a standard anterior portal, but 42% of the ramp lesions were apparently missed, and were only discovered by probing the tear through a posteromedial portal ‘after minimal debridement of a superficial soft tissue layer with a motorized shaver’ (i.e. a pretty invasive approach). [Ref 2] Furthermore, it has also been stated that ramp lesions can only be treated effectively by suturing via a posteromedial accessory portal using mini aneurysm-type needles, such as the Arthrex QuickPass lasso. [Ref 3]
The above suppositions are, however, false, and are simply not the case!…
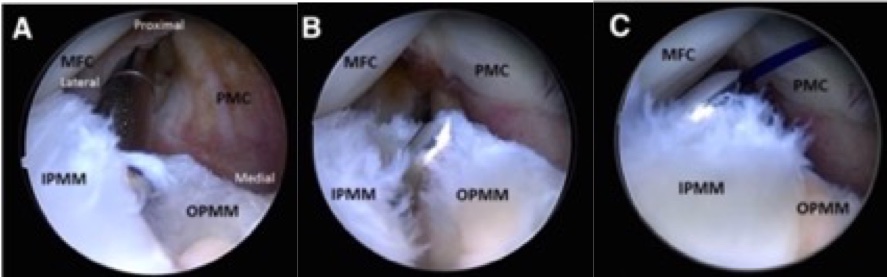
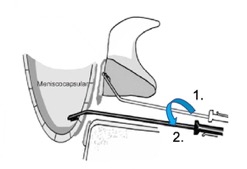
Access to the posterior aspect of the medial compartment can often be tight and restricted, making clear visualisation difficult. However, even when visualisation is poor, it is nearly always possible to pass an arthroscopic probe under the posterior horn of the medial meniscus. If the posterior meniscocapsular attachment is intact, then the probe hits a firm stop and the hook cannot be rotated up (proximally) behind the bulk of the tissue of the meniscal posterior horn. If, however, there is a ramp lesion present, then the tip of the probe can be rotated and passed posterior to the posterior horn, ‘catching’ the posterior horn as one pulls anteriorly. Therefore, even if a ramp lesion cannot be visualised from the front of the knee via standard portals, it can be felt.
If there is any suspicion of a ramp lesion but if visualisation and access are actually restricted, then one should have a very low threshold for proceeding with pie-crusting of the MCL.
Pie-crusting of the MCL is performed percutaneously with a needle, and involves making multiple tiny perforations in the medial collateral ligament and mainly in the posterior oblique portion of the medial tissues. This is best done with the knee at about 20 degrees of flexion under a valgus force. As the medial tissues ‘give’ there is a palpable (and sometimes audible) tearing of the tissues and the medial compartment opens up further by just a few additional millimetres. This makes a massive difference and allows radically improved visualisation and access to the whole of the posterior portion of the medial compartment.
If there is any kind of tear in the posterior horn of the medial meniscus, then this can then be seen, probed and dealt with far more easily and with a much lower risk of A) missing the true extent of a tear, B) missing a tear altogether, C) failing to deal fully and sufficiently with whatever tears might be present, or D) scuffing and damaging the articular cartilage on the surface of the medial femoral condyle by struggling to gain sufficient access. Once the MCL has been pie-crusted, it is then far easier to feel (with the arthroscopic probe) and actually see and then deal with a ramp lesion.
Research has shown that the MCL heals very well indeed after pie-crusting (just like a minor partial MCL tear / sprain), with no residual valgus laxity in the joint and with no adverse long-term sequelae. As stated above, the threshold for pie-crusting the MCL should be very low. [Ref 4]
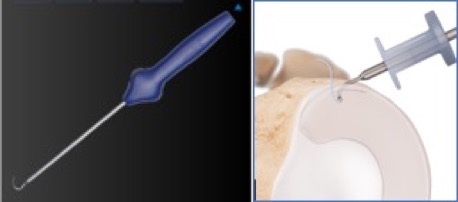
Once a ramp lesion has been identified, it is then relatively easy and straight forward to repair the tear, and this absolutely can be performed using an all-inside technique via standard anteromedial and anterolateral portals. However, what is required is an all-inside meniscal suturing device that is reliably bendable, which is where the Stryker AIR+ device really comes into its own…
The Stryker AIR+ device can be bent pretty much to 90 degrees, if necessary, without adversely affecting the deployment of its anchors. Not only does this allow all-inside repairs all the way round to the region of the junction of the anterior horn and body portions of a meniscus, it also makes the AIR+ ideal for repairing ramp lesions.
The distal end of the AIR+ device is bent to about 30 to 45 degrees at a point about 2cm or so from its tip. This allows the needle to be placed through the tibial under-surface of the meniscus and passed ‘up’ (proximally) as well as ‘back’ (posteriorly), with the anchor being deployed on the posterior surface of the posterior horn. The AIR+ is then rotated 180o so that the bent distal end is facing ‘downwards’ (distally). The second anchor can then be deployed firmly into the posterior capsule / meniscotibial ligament tissue just distal to the surface level of the medial tibial plateau. (It is important that this is done using the depth guard for the needle set at a maximal depth of 1cm and with the knee in relative flexion rather than relative extension, and with the tip of the needle angled slightly medially rather than towards the midline, in order to try and minimise the potential risk of neurovascular damage to the popliteal neurovascular bundle.)
Next, it is important to place a series of 3 or 4 sutures on the tibial under-surface of the posterior horn but without actually tightening any of the sutures. This maintains access. As soon as the first suture is tightened, the posterior horn comes down quite firmly onto the surface of the medial tibial plateau, making further visualisation and access much more difficult. Therefore, the sutures should be placed sequentially and then subsequently tightened and cut sequentially.
The stability of the posterior horn can then be assessed. If necessary, further sutures can then be placed on the femoral surface of the posterior horn, sometimes with a combination of vertical sutures through the meniscus and the posterior capsule around the rim of the posterior horn, and, if required, 1 or 2 additional horizontal or oblique sutures to help the posterior horn sit down neatly and firmly.
The above technique gives a very solid stable fixation that is technically easier and quicker than attempting to suture the meniscotibial ligament via an accessory medial portal, and with stronger tighter sutures.
KEY POINTS
- Meniscal ramp lesions are a common finding in ACL-deficient knees.
- Ramp lesions can sometimes be seen on MRI, but are often missed.
- One should always have a very low index of suspicion for there potentially being a ramp lesion present in every ACL-deficient knee and at the time of every ACL reconstruction.
- Even with poor access, a ramp lesion can pretty much always be felt (even if not seen) with an arthroscopic probe from standard anterior portals.
- Have a very low threshold for pie-crusting the MCL if visualisation and access to the posterior aspect of the medial compartment are in any way suboptimal.
- One the MCL has been pie-crusted, it becomes easy to see and deal with tears in the posterior horn of the medial meniscus, including ramp lesions.
- Ramp lesions can be repaired with a simple easy all-inside technique via standard anteromedial and anterolateral arthroscopy portals, but it requires an all-inside meniscal repair device that is bendable: i.e. the Stryker AIR+.
- An accessory posteromedial portal with shaving of the posteromedial tissues is NOT a necessary requirement for repairing ramp lesions.
- Sutures through the tibial under-surface of the posterior horn of the medial meniscus should be placed sequentially and then subsequently tightened and cut sequentially, before then placing any sutures that might be required on the superior (femoral) surface of the posterior horn.
- A firm solid repair can be achieved safely and reliably with multiple sutures using the Stryker AIR+ device, simply by ensuring adequate visualisation and access, and by appropriately bending the end of the needle.
Video of surgical technique
Watch a video of the surgical technique for the repair of a medial meniscal ramp lesion using Stryker AIR+ meniscal repair sutures:
References
- Strobel M.
Manual of Arthroscopic Surgery.
New York, NY: Springer; 1988. - Sonnery-Cottet et al.
Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee.
Am J Sports Med, 2014
https://pubmed.ncbi.nlm.nih.gov/24567252/ - Repair of Meniscal Ramp Lesions Through a Posteromedial Portal During Anterior Cruciate Ligament Reconstruction: Outcome Study With a Minimum 2-Year Follow-up.
Thaunat et al (incl. Sonnery-Cottet)
Arthroscopy, 2016
https://www.arthroscopyjournal.org/article/S0749-8063(16)00249-8/abstract - Need Room to Operate? Partial and Intentional Release of the Knee Medial Collateral Ligament for Medial Meniscal Surgery.
Lubowitz et al
Arthroscopy, 2020
https://www.sciencedirect.com/science/article/abs/pii/S0749806320303315