Douchebag doctor of the week: Episode 3.
Hello campers. Episode 3 of ‘Douchebag doctor of the week’ is here, and this one’s a ‘good’ (bad!) one…
Case history.
A 38-year-old man came to clinic recently complaining of couple of years’ history of gradually worsening right anterior knee pain, with pain on stairs and ladders, and pain with kneeling or squatting; however, the patient was relatively fine walking on the flat, and he was still able to manage any distance (i.e. typical patellofemoral symptoms). The patient was unable to run (although this was because of pre-existing hip problems, from FAI).
On examination, the patient’s knee had a full and pain-free range of motion. The patellar tracking looked good, but the patella was prominent, and it did not seem to engage firmly into the trochlear groove until about 60 degrees of knee flexion. The patella was quite mobile laterally with the knee in extension and the quads relaxed, but the patellar apprehension test (for potential instability) was negative. There was slight crepitus in the patellofemoral joint with knee movements, and a Clark’s test for patellofemoral irritability was mildly positive.
The patient had already been to see a well-known surgeon in one of our two most internationally famous university cities. (From my experience, these two universities tend to churn out individuals whose intellectual arrogance is writing cheques that their ability for independent critical thinking and their EQs just can’t cash – but that’s probably for a different blog!) This surgeon advised the patient that he could have either PRP injections into his knee, or that alternatively, he could have articular cartilage grafting on the back of his patella.
I reviewed the patient’s MRI scan with him. This showed:
– normal medial and lateral compartments, and all the ligaments were intact,
– patellar dysplasia,
– no significant trochlear dysplasia,
– good patellar tracking (with the knee in extension),
– a well-placed tibial tuberosity, with a normal TTTG distance,
– the medial retinaculum was intact and there was no evidence of any traumatic damage to the medial-most edge of the patella (i.e. there was no radiological evidence to suggest that there had ever been any patellar dislocations in the past),
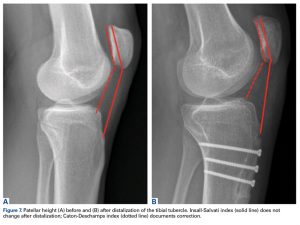
– there was clear evidence of patella alta (with an increased Insall-Salvati ratio and a decreased patellotrochlear index,
– there was just slight increased signal in the articular cartilage on the back of the patella (i.e. early wear and tear, or, to use the somewhat old-fashioned term: ‘chondromalacia patellae’), but with no significant fissures or flaps, and with no actual cartilage loss at all, and certainly with no areas of any full-thickness loss with any actual bare bone exposed.
My advice to the patient was that if he felt that his anterior knee pain and his functional restrictions were genuinely bad enough to justify the not-inconsiderable pain, hassle and risks of the surgery, then he could have a tibial tuberosity advancement osteotomy, to correct his patella alta (but without the need for this to have to be combined with an arthroscopy of the knee as well, at the same time).
I reassured the patient that there was certainly no indication whatsoever for any kind of articular cartilage grafting type procedure in his knee, and I also explained to the patient that in my opinion, having PRP injections into his knee would be completely pointless.
I e-mailed the patient a load of information to read about patella alta and about tibial tuberosity advancement osteotomy surgery, and at the time of writing this, the patient is currently mulling things over.
So… main points that stood out to me:
1. The first surgeon that this patient saw didn’t explain to him that he had patella alta.
2. The surgeon offered the patient PRP injections.
3. The surgeon also offered the patient surgery, with articular cartilage grafting (of some kind) to his patella, when the patient doesn’t actually even have any articular cartilage loss on the back of his patella!
Questions for the audience:
1. Should I name the surgeon? (With time, some of you may actually eventually start to appreciate that this question is stated in an ironically rhetorical fashion!) 😉
2. Is this surgeon the biggest ‘Douchebag of the week’ so far?
3. Sadly, I’ve got yet more of these ‘horror story’ cases lined up – so, do you actually find these blogs useful, and would you like to me to continue?
Epilogue for some of my esteemed colleagues
I’ve heard that this ‘Douchebag doctor of the week’ has apparently stirred up some discussion and ruffled some feathers within the ranks of some of my esteemed colleagues here in my sunny hometown of London – if you’re one of these individuals, and if for some reason these stories (every one of which is, sadly, real and absolutely true!) in some way offend you… then A) is it potentially because you maybe recognised some of your own traits and behaviours in some of these stories? or B) do you believe that good doctors should simply keep quiet and that we shouldn’t actually warn people about some of the poor behaviour of some of the bad doctors, and C) if you don’t appreciate these blogs, then why on Earth are you actually bothering to read them? – please, just do us both a favour and please just go away.
Love & Light.
Ian