I’m ‘excited’ about this ‘Douchebag’ story – because this time we’ve got a special guest: the patient’s physio!
Luckily, this patient was fortunate enough to have a physio who’s senior enough, confident enough and decent enough to stand up against a very senior consultant by raising a red flag and encouraging the patient to get a second opinion.
Personally, I was shocked and appalled (again!) by what this patient told me. What do you think?….
Case History
History
An 86-year-old gentlemen was complaining of gradually increasing pain and stiffness in his thigh muscles, with increasing difficulty walking.
He went to see a Professor of Orthopaedics at an internationally famous and very flash clinic / hospital in Central London. The patient was listed for bilateral simultaneous knee replacement surgery.
As noted above, the patient’s physio was deeply concerned about this proposed plan of action, and hence he asked me to see the patient for a second opinion. At the time that I saw the patient in clinic he was, at that point, booked in to have this surgery just the following week.
When I called the patient’s name for him to come into my consulting room from the waiting area, it took the patient a while to get up from his seat, and it took him a while to get going… before he was then able to walk into my room reasonably well.
The patient said that he had pain in his knees that tended to come and go, but at worse, it was only “moderate” in severity. The patient felt this pain mainly on stairs, and he therefore tended to go up and down stairs just one step at a time. However, the patient was still able to go out for his usual ½-hour walk every day. Importantly, he stated that when he starts to walk he feels very stiff and he finds it difficult to get going; however, as he gets going his muscles then start to feel better, and that he then feels more mobile and a lot better. The patient was not having to take any painkillers or anti-inflammatories, and his knees were not affecting his sleep. The patient stated that he was not doing any other exercise at all apart from his usual ½-hour once-a-day walk.
Unfortunately, the patient had a long list of medical problems, including atrial fibrillation (for which he was on blood thinners), major bowel issues (with colitis, and with him having had a colostomy), hypertension and prostate issues. Of note (and as so often seems to be the case nowadays), as well as being on a long list of medications, the patient was also on statins for his cholesterol.
Examination
When I examined the patient’s knees, there was a slight varus in both knees. There was no tenderness to palpation around either knee and there was no effusion on either side. Both knees had full extension. The patient was able to flex each knee up fully, with no pain with deep flexion. Both knees were stable. A McMurray’s test was negative on both sides. The patellar tracking at the front of each knee looked central and a Clark’s test for patellofemoral irritability was negative at the front of each knee.
Both hips had a good range of motion, and there was no pain with hip movements, and the patient had a reasonable range of motion in his back, with no back pain, and with no abnormal neurological signs.
When I asked the patient to localise his pain, he very specifically rubbed his thigh muscles up and down, and he localised his pain to his quads muscles.
Imaging
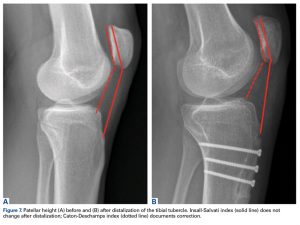
The patient had had some X-rays, and I reviewed these with him: they showed evidence of moderate OA in the medial compartment of each knee, with fully-blown patellofemoral OA at the front of both knees.
Summary
So, what was the problem with the treatment plan of the previous consultant?
First, knee replacement surgery is a big deal. It’s a really big painful operation with very difficult post-op rehab afterwards, and with significant potential risks. When it goes well, the results can be great, but when there’s a problem, it can be catastrophic.
If a patient is ‘young’ (which is very much just an arbitrary concept), then we try to avoid knee replacement if possible (unless it’s a last resort), because the younger a patient is when they have a knee replacement, the bigger the risk of it failing (wearing out) and ending up needing a re-do (a revision knee replacement) within their time. Revision knee replacement is twice as big/complex as a primary, with double the potential complication risk, with slower recovery, with poorer outcomes and with higher re-revision rates. However, if you perform knee replacement surgery in someone in their 70’s, then the risk of them ending up needing a revision within their lifetime is only about 10%, and in about 90% of patients the prosthesis will end up outlasting them.
With older patients, however, the focus often tends to be more on the potential associated risks of the surgery… The older one is, and also the more medical problems one has, then the lower one’s physiological reserve is, in terms of whether the patient is likely to be able to cope with the actual surgery itself. Also, the older one is and the weaker one is, then the less likely they are to be able to cope with the extensive difficult post-op rehab that’s required after knee replacement surgery – and if you don’t do the proper rehab after a knee replacement, then you’re far less likely to end up with a good outcome (i.e. there’s a higher risk of the patient ending up with a stiff and painful knee, with them ending up very unhappy indeed).
It’s hard enough to do the rehab after single unilateral knee replacement surgery. It’s doubly hard to do sufficient rehab if you have both knees done together, at the same time.
Next, this patient was booked in for major surgery very quickly indeed, with minimal time to think things over, to do his own reading or to ask questions, and certainly with no time to do any prehab.
Personally, I always advise my patients to do as much prehab as they possibly can ahead of any knee replacement surgery. Importantly, the fitter and stronger a patient can get themselves ahead of any knee replacement surgery, then the better they’re likely to cope with the op and with the post-op rehab afterwards. Also, if a patient does really well with their prehab, and if they actually end up doing so well that they’re feeling significantly better… then they might even end up not actually needing / wanting the surgery (or at least not, perhaps, for a while longer).
Next, and very importantly… this patient’s main complaint (if you cared to ask the right questions and actually listen properly to what he had to say) was of muscle pains and stiffness, and in clinic he was repeatedly rubbing and massaging specifically his quads muscles.
OK, the patient’s X-rays showed medial plus patellofemoral OA in both knees; however, when I examined the patient’s knees, both knees had a full and pain-free range of motion. Yes, the patient was complaining of pain on stairs, and he was having to go up and down stairs just one step at a time; however, the patient’s patellar tracking looked central and his Clark’s test for patellofemoral irritability was negative at the front of each knee.
Importantly, one should treat the patient, not just the imaging!
The key potential culprit that jumped out at me when I saw this patient in clinic was that he was on statins!
Statins are well-known (or, at least well-known by anyone who actually cares to read the warning inserts that come with every box of tablets, which list the potential side effects) to cause muscle pains, muscle stiffness and muscle weakness … all of which match the exact complaints of this specific patient.
My proposed plan of action
So, what was my advice to this patient?….
- First, I advised the patient to cancel (or at least postpone) the surgery that was booked in for him for the following week.
- I e-mailed the patient a copy of his clinic letter, which was 4 sides of A4.
- I e-mailed the patient links to some additional specific articles that I wanted him to read:
– knee arthritis: https://kneereplacements.co.uk/knee-arthritis/
– the conservative management of the symptoms of knee arthritis: https://kneereplacements.co.uk/non-surgical-treatments/
– knee replacement surgery: http://kneereplacements.co.uk/knee-replacement-surgery-performed/
– the risks of knee replacement surgery: https://kneereplacements.co.uk/potentials-risks-possible-complications-knee-replacement-surgery/
– the timing of when to actually go ahead with knee replacement surgery: http://kneereplacements.co.uk/right-time-go-ahead-knee-replacement-surgery/
- I advised the patient to go through all of this information carefully, and then to e-mail me back with whatever potential further questions he might have.
- The patient had a treadmill, a rowing machine and an exercise bike at home; however, he hadn’t used these for a very long time. So, I advised the patient to start using his exercise bike for 20 to 30 mins a day, every day, and I also advised him to go back to his physio for some additional, more-detailed exercise advice, and I advised the patient to commit to a course of rehab treatments.
- Finally, I advised the patient to stop his statins for a trial period.
I also advised the patient to get himself a copy of this book and to read it carefully:
A Statin-Free Life, by Dr Asseem Malhotra, Consultant Cardiologist
https://www.worldofbooks.com/en-gb/products/statin-free-life-book-aseem-malhotra-9781529354102
I’ve asked the patient to drop me an update in 2 months’ time, to let me know how he is getting on.
Comments from the patient’s physio:
“The patient was initially presented to me by an experienced personal trainer colleague who expressed concerns about her client’s recommendation for bilateral total knee replacement surgery by a Consultant Orthopaedic Knee Surgeon. She sought physiotherapy input to gain a more comprehensive perspective regarding the patient’s suitability for surgery.
The patient is an 86-year-old male with imaging-confirmed bilateral knee osteoarthritis, currently under consultant care. Historically, he reported intermittent knee pain, with no recent changes in intensity or frequency. However, he clearly described a significant decline in his physical capabilities, notably struggling with walking and performing sit-to-stand movements from chairs, beds and toilets. He acknowledged never having engaged in regular physical activity, and expressed a dislike for exercise.
Clinical examination revealed a full, pain-free range of motion in both knees, and no tenderness upon joint-line palpation. No swelling, effusion, or ligamentous instability was detected. However, he demonstrated substantial bilateral quadriceps muscle weakness, unable to complete the sit-to-stand test without arm support, performing far below the recommended 8-14 repetitions in 30 seconds for his age group.
My assessment concluded that the patient’s primary issue is significant lower limb muscle weakness and overall physical deconditioning rather than joint pathology alone. Consequently, I recommended against the proposed bilateral knee replacement surgery at this stage, due to his poor physical condition. Instead, I advised a three-month intensive rehabilitation program, aimed at improving muscle strength and functional capacity. This strategy would either eliminate or significantly delay the need for surgical intervention, and, importantly, optimise his physical condition should surgery become necessary later.
In reflecting upon this case, I believe the initial surgical recommendation lacked a comprehensive evaluation of the patient as a whole. Critical factors such as his physical fitness, medical history, and social circumstances were not sufficiently considered. The patient currently supports his wife, who requires daily external care, further complicating his situation. Given his marked sarcopenia, undergoing double knee replacement surgery would likely severely compromise his mobility, potentially rendering him bedridden and significantly diminishing his long-term quality of life. Furthermore, the absence of pre-operative rehabilitation planning exacerbates the risk of poor post-operative outcomes.
Lastly, considering the patient’s advanced age, historical aversion to physical activity and existing responsibilities, he appeared to be a poor candidate for such extensive surgical intervention without significant preparatory measures.
Although the patient had been recommended for surgery by a well-known surgeon, I tried to put that aside and look at this patient’s case objectively and without bias. Because my viewpoint was that the patient was not surgically appropriate, I sought a second surgical opinion and referred the patient across to Mr Ian McDermott, who I knew would look at the scenario properly, in detail, considering all of the variables.”
QUESTIONS
So, questions for you….
- Do you think that it’s appropriate / sensible to offer a relatively frail 86-year-old gentleman with a long list of medical problems bilateral simultaneous knee replacement surgery?
- Do you think it’s appropriate to book a patient in for very major surgery in such a short timeframe, with them not being given much time at all to think things over or do any prehab?
- Do you think it’s appropriate for the patient to have his statins stopped for a trial period?
- Would you like to know who this surgeon was and where he’s based?
And finally….
A very big ‘well done’ and ‘thank you’ to the patient’s physio, who was brave enough and confident to stand up for his patient and do the right thing by ‘daring‘ to question the opinions, decisions and actions of one of London’s most ‘famous’ knee surgeons. And if that surgeon doesn’t deserve the title of ‘douchebag’, then perhaps you might like to propose some alternative titles that you think might potentially suit better??…